Notifications for Providers
Several times a year, Highmark notifies providers of important policies and guidelines. The following notification is for your information and reference.
Reimbursement, Claims & Billing
New and updated reimbursement policies
Highmark regularly issues new or updated reimbursement policies. Keep an eye on the Provider Resource Center Home Page for eBulletins announcing new policies and the Reimbursement Policy page for policy updates.
To access Highmark reimbursement policy bulletins, select CLAIMS, PAYMENT & REIMBURSEMENT from the Provider Resource Center main menu, and then click on Reimbursement Policy.
Watch for Updates to Highmark’s List of Procedures Requiring Authorization
During the year, Highmark adjusts the List of Procedures and Durable Medical Equipment (DME) Requiring Authorization, which includes outpatient procedures, services, DME, and drugs that require authorization for our members.
These changes are announced in the form of Special eBulletins that are posted on Highmark’s Provider Resource Centers (PRC).
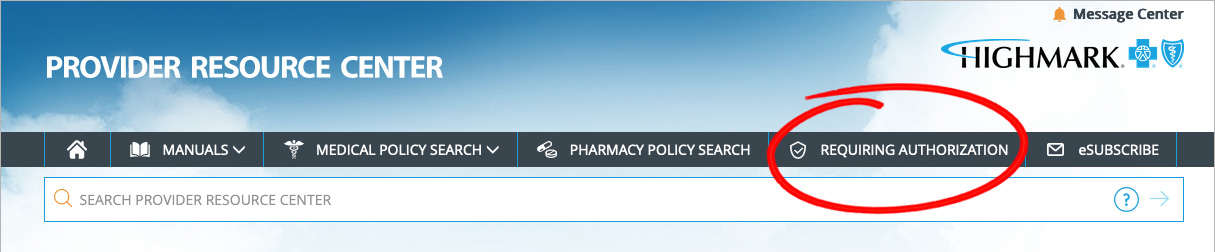
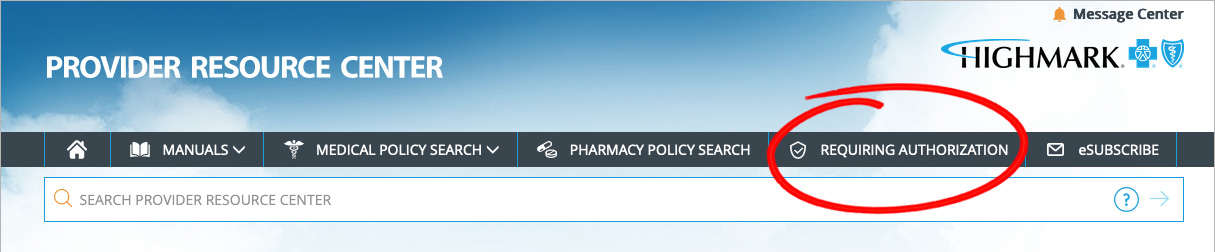
To view the List of Procedures/DME Requiring Authorization, click Requiring Authorization in the gray bar near the top of the PRC homepage.
Please note that the Highmark member must be eligible on the date of service and the service must be a covered benefit for Highmark to pay the claim.
You may use NaviNet or the applicable HIPAA electronic transactions to:
- Check member benefits and eligibility
- Verify if an authorization is needed
- Obtain authorization for services
If you are not signed up for NaviNet or do not have access to the HIPAA electronic transactions, please call Clinical Services to obtain an authorization for services:

Provider News, Issue 3, 2021 | © 2021 Highmark Blue Cross Blue Shield
 Please note that the Highmark member must be eligible on the date of service and the service must be a covered benefit for Highmark to pay the claim.
You may use NaviNet or the applicable HIPAA electronic transactions to:
Please note that the Highmark member must be eligible on the date of service and the service must be a covered benefit for Highmark to pay the claim.
You may use NaviNet or the applicable HIPAA electronic transactions to: