Authorization Updates
 During the year, Highmark adjusts the List of Procedures and Durable Medical Equipment (DME) Requiring Authorization. For information regarding authorizations required for a member’s specific benefit plan, providers may:
During the year, Highmark adjusts the List of Procedures and Durable Medical Equipment (DME) Requiring Authorization. For information regarding authorizations required for a member’s specific benefit plan, providers may:
- Call the number on the back of the member’s card,
- Check the member’s eligibility and benefits via NaviNet®
 , or
, or
- Search BlueExchange through the provider’s local provider portal.
These changes are announced in the form of Special eBulletins that are posted on Highmark’s Provider Resource Center (PRC).
The most recent eBulletins regarding prior authorization are below:
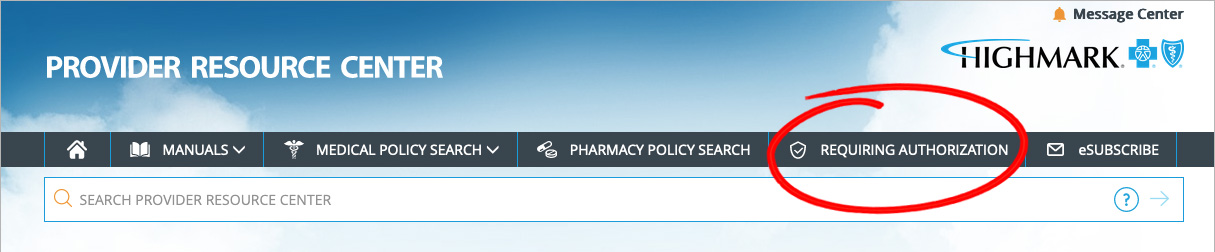
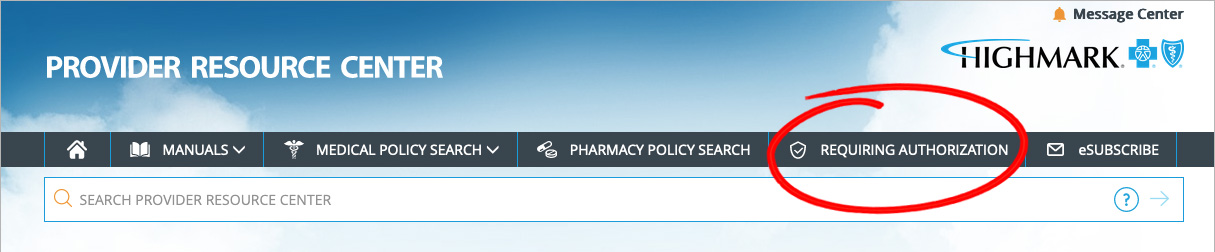
To view the List of Procedures/DME Requiring Authorization, click Requiring Authorization in the gray bar near the top of the PRC homepage.
Please note that the Highmark member must be eligible on the date of service and the service must be a covered benefit for Highmark to pay the claim.
NaviNet®  is the preferred method for:
is the preferred method for:
- Checking member benefits and eligibility
- Verifying whether an authorization is needed
- Obtaining authorization for services


Provider News, Issue 5, 2022 | © 2022 Highmark Blue Cross Blue Shield

 During the year, Highmark adjusts the List of Procedures and Durable Medical Equipment (DME) Requiring Authorization. For information regarding authorizations required for a member’s specific benefit plan, providers may:
During the year, Highmark adjusts the List of Procedures and Durable Medical Equipment (DME) Requiring Authorization. For information regarding authorizations required for a member’s specific benefit plan, providers may:
 , or
, or



 is the preferred method for:
is the preferred method for: