
 During the year, Highmark adjusts the List of Procedures and Durable Medical Equipment (DME) Requiring Authorization. For information regarding authorizations required for a member’s specific benefit plan, providers may:
During the year, Highmark adjusts the List of Procedures and Durable Medical Equipment (DME) Requiring Authorization. For information regarding authorizations required for a member’s specific benefit plan, providers may:
 or NaviNet®
or NaviNet® , or
, orThese changes are announced in the form of Special Bulletins and other communications posted on Highmark’s Provider Resource Center (PRC). The most recent updates regarding prior authorization are below:
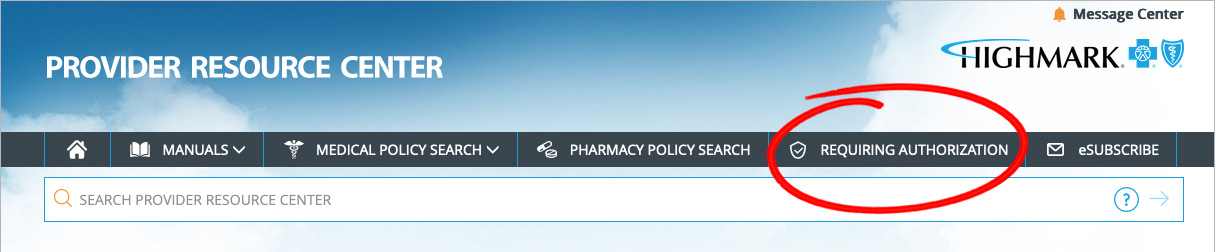
To view the full List of Procedures/DME Requiring Authorization, click REQUIRING AUTHORIZATION in the gray bar near the top of the PRC homepage.
Once redirected to the Procedures/Service Requiring Authorization page, click View the List of Procedures/DME Requiring Authorization under PRIOR AUTHORIZATION CODE LISTS.
Please note that the Highmark member must be eligible on the date of service and the service must be a covered benefit for Highmark to pay the claim.
Availity or NaviNet
or NaviNet is the preferred method for:
is the preferred method for: